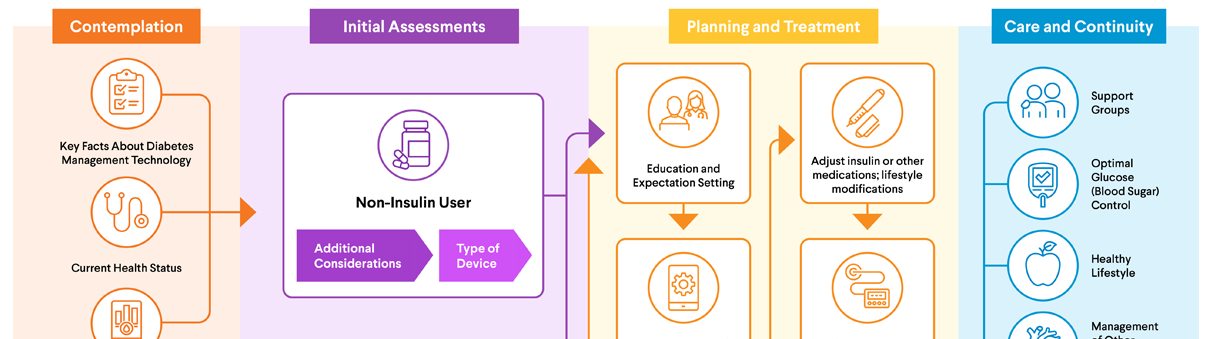
Planning & Treatment
Care & Continuity

Care & Continuity
Living with diabetes can be overwhelming at times. Keeping track of your blood sugar (glucose), taking insulin and/or diabetes medications, keeping your diabetes technology devices in good working order, and trying to make healthy lifestyle choices might make you feel like managing diabetes is a full-time job.
While it's true that diabetes management takes time and effort, it becomes easier once you start building healthy habits and working diabetes care into your everyday routine. What's more, taking time to care for yourself and your diabetes can pay off for your health. Making healthy choices can lower your risk of developing diabetes-related complications, such as problems with your eyes, heart, nerves, or kidneys. Healthy daily habits can also improve your overall health and help you feel your best.
You have diabetes, but it doesn't define you. In fact, you have the power to achieve success in diabetes self-care and live well. By taking the following steps, you can boost your health and quality of life.
 Support Groups
Support Groups
Living with diabetes may be challenging at times. Although friends and family may be sympathetic, having the support of other individuals with diabetes is especially helpful. Peer-to-peer support may help you navigate the world of diabetes self-care and may help you learn new ways to cope with and manage diabetes.
Support groups offer you the chance to be part of a community of peers facing similar challenges as you. These groups are a great resource for emotional support, informational education, practical advice, motivation, and empowerment. You can also support each other as you learn how to manage your diabetes and use various types of diabetes technology.
Here's a list of patient support groups for you to consider:
- DiabetesSisters: This nonprofit organization provides support and education for people with diabetes.
- Beyond Type 1: This nonprofit organization changing what it means to live with diabetes. Through platforms, programs, resources, and grants, Beyond Type 1 is uniting the global diabetes community and providing solutions to improve lives today.
- Beyond Type 2: Beyond Type 2 is a place for everyone impacted by type 2 diabetes to share their stories, get connected to the community, and find resources on topics from daily management to mental health.
- Defeat Diabetes: For nearly 30 years, the Defeat Diabetes Foundation has supported research-based and sustainable solutions aimed at preventing, identifying and managing type 2 diabetes.
- Diabetes Link: The Diabetes Link is the go-to for peer support, resources, and leadership opportunities designed specifically for young adults.
- JDRF: This organization is improving lives today and tomorrow by accelerating life-changing breakthroughs to cure, prevent and treat type 1 diabetes and its complications.
- The diaTribe Foundation: Aims to help individuals and caregivers better understand diabetes and make healthy choices.
- Children's Diabetes Foundation: The fundraising arm of the Barbara Davis Center for Diabetes, this organization focuses on patient support, awareness, and research.
 Optimal Blood Sugar (Glucose) Control
Optimal Blood Sugar (Glucose) Control
Your health care professional will talk with you about your target blood sugar range. This is the blood sugar level your health care professional believes is best for you.
Keeping your blood sugar in the recommended target range as much as possible helps lower your risk of developing diabetes-related complications. These complications, including problems with your eyes, heart, nerves, and kidneys, can become quite serious. For example, frequently out-of-range blood sugar can lead to vision loss or even blindness.
For more information on hypoglycemia (low blood sugar) and diabetic ketoacidosis (result of high blood sugar) visit our insulin user page here.
To learn more about hypoglycemia (low blood sugar) for people who do not use insulin, visit our non-insulin user page here.
In addition, keeping your blood sugar in range may help you feel better. For many people, in-range blood sugar is linked to:
- Better energy levels
- Better mood
- Fewer infections
- Greater ability to heal
- Less hunger and thirst
- Less need to urinate frequently
Health care professionals typically give non-pregnant adults with diabetes two different blood sugar targets:
- One for before a meal (usually between 80 and 130 mg/dL)
- One for two hours after a meal (usually less than 180 mg/dL)
Some health care professionals suggest lower blood sugar targets (under 110 mg/dL before a meal and under 140 mg/dL two hours after a meal). And many recommend that blood sugar fall between 70 and 180 mg/dL for approximately 70% of the day if it can be achieved safely without causing hypoglycemia (low blood sugar). You can work with your health care professional to determine what blood sugar target ranges are best for you.
Blood sugar targets are not one-size-fits-all. Your personal blood sugar target ranges may vary based on factors such as your age and other conditions you have. For example, blood sugar targets may be stricter during pregnancy and less strict for people with a higher risk of complications from low blood sugar.
You can track your blood sugar levels by testing regularly with a standard glucometer that measures the blood sugar from a finger-prick blood sample. Or you can use a continuous glucose monitor (CGM) system. Note: Although they may be referred to as blood sugar monitors, CGMs actually measure the glucose (sugar) in the fatty tissue in your body, rather than your blood.
One of the benefits of using a CGM device is that it measures, stores, and transmits blood sugar data on a regular basis and can notify you if your blood sugar is too high or too low, or is trending up or down.
Some good ways to keep your blood sugar within your recommended target ranges include following your diabetes-friendly eating plan, exercising regularly, and taking insulin and/or other diabetes medications as recommended by your health care professional.
You may notice that other things besides eating and exercise affect your blood sugar. For example, your blood sugar may go up or down when you are tired, skip meals, or experience stress. By tracking your blood sugar over time, you can learn about what causes your blood sugar to go above or below your target. Armed with this information, you can then make informed decisions.
If you are having trouble staying within your recommended target blood sugar ranges, talk with your diabetes care team. They may be able to recommend lifestyle changes, medication changes, or diabetes technology devices that can help.
Visit our AACE Prescription Affordability Resource Center for affordability assistance.
 Healthy Lifestyle
Healthy Lifestyle
Practice Healthy Diabetes Hygiene
People with diabetes have a higher-than-average risk of developing various types of infections because of the effect diabetes can have on your immune system and your body's inflammatory responses.
Keeping your blood sugar in your target range as much as possible can help your body fight infection. You can also help protect yourself by following these hygiene guidelines:
- Avoid walking barefoot to protect yourself from foot infections
- Contact your health care professional if you have a wound that isn't healing, a fever over 101°F, urinary tract itching or increased urination, or any other signs of infection.
- Eat a healthy diet, including high-fiber, nutrient-rich fruits and vegetables.
- Exercise regularly and get enough sleep.
- Manage stress through mindfulness, behavioral therapies, and mental health counseling and treatments.
- Follow your diabetes care team's recommendations for good hygiene and infection prevention related to finger-prick blood testing, injecting insulin, and care and maintenance of your CGM and insulin pump (if you use them).
- Keep your vaccinations up to date.
- Take good care of your teeth by brushing and flossing regularly and seeing your dental care professional as often as recommended.
- Wash your hands often and use hand sanitizer.
- Wear well-fitting socks and shoes to prevent blisters and sores on your feet.
Eat a Healthy Diet
Following a diabetes-friendly eating plan is one of the best things you can do to manage your diabetes and support your overall health. Eating nutrient-rich foods in amounts that are ideal for you helps minimize the spikes in blood sugar after meals and can reduce the need for increased medications or insulin doses. It can also lower your risk of a variety of other health conditions, including heart disease, some types of cancer, and obesity.
Your diabetes care team can guide you in creating a meal plan that meets your needs. In general, a healthy diabetes eating plan focuses on the following:
- Foods that are good for your health: These include vegetables, fruit, whole grains, lean meats and fish, low-fat dairy, beans and peas, nuts, seeds, and healthy fats. Healthy foods are rich sources of important nutrients such as vitamins, minerals, and compounds that help your body fight disease.
- The right amount of food: Eating just-right portion sizes can help with blood sugar control as well as weight management.
- Whole foods rather than processed foods: For example, eat an apple rather than drinking apple juice, as whole foods tend to raise blood sugar less or more slowly than processed foods.
- Fewer foods that can have a negative impact on your health: These include fried foods, foods that contain a high content of saturated fats (such as red meat and processed meats), foods that are high in sodium (salt), sugar-sweetened and artificially sweetened drinks, and sweets.
- Foods that are low in added sugars and starches: Sugary foods (such as cake, cookies, and candy) and starchy foods (some kinds of breads, cereals, snack foods, and even some types of vegetables and fruits) can raise your blood sugar more or faster than foods that are lower in sugar and starch.
- Foods that are higher in fiber: Eating fiber-rich foods can help prevent spikes in blood sugar and reduce the risk of cardiovascular disease. The recommended total dietary fiber intake per day for an average adult is 22-34 grams. The best sources of fiber are plants including vegetables and fruits.
- Whole grains rather than refined grains: For example, eat whole wheat bread rather than white bread.
- Healthy, natural carbohydrates: Glucose is the most essential fuel for every cell in your body. Starches are an essential nutrient requirement for a healthy diet. However, imbalanced intake of high and processed carbohydrates, such as fast food, can have an unhealthy effect on your blood sugar levels. Therefore, try to choose smaller portions of nutrient-rich natural starches, such as sweet potatoes or other root vegetables that support a healthy stomach and gastrointestinal tract. Another source of healthy starches includes beans, which are an excellent source of essential vitamins, nutrients, protein, and carbohydrates. The timing of food consumption can also affect your blood sugar levels. Make sure to avoid large portions or late-night eating that can contribute to higher blood sugar levels throughout the nighttime.
- The right amount of carbohydrates: Carbs in food are measured in grams. A diabetes-friendly diet usually focuses on limiting how many grams of carbs you eat at each meal and eating about the same number of carbs at each meal. Your diabetes care team can teach you about "carbohydrate-counting," which is a process of counting and tracking the carbohydrates you eat throughout the day.
- Regular mealtimes: Maintaining a consistent schedule for meals helps keep blood sugar levels in check. Skipping meals may increase your risk for low blood sugar and may also result in a slower metabolism over time. Talk with your health care professional about the ideal personalized approach to scheduled mealtimes for you.
Did You Know?
Diabetes and Healthy Eating
- You can still eat the foods you enjoy when you have diabetes. However, to help keep your blood sugar in range, you may need to limit portion sizes or how often you eat certain foods.
- A registered dietitian, diabetes educator, or other health care professional with nutrition training can work with you to create a meal plan that aligns culturally and with your budget to help keep your blood sugar in range.
- If you have diabetes, your health insurance may pay for medical nutrition therapy (MNT). (For example, Medicare covers MNT for those who qualify.) MNT is nutrition care provided by a registered dietitian nutritionist. It includes education, advice, and follow-up care centered around healthy eating and behavior changes. Ask your health care professional about whether MNT is right for you.
Take Advantage of Nutritional Support Resources
When it comes to planning a diabetes meal plan, you aren't not alone. Your diabetes care team can help. In addition, many health insurance plans, including Medicare, pay for MNT.
Here's something important to keep in mind: A diabetes-friendly approach to nutrition doesn't mean you have to give up all the foods that you love. As you work with your diabetes care team to create your meal plans, tell them about foods that are important to you so you can learn how to include them in your diet.
Eating a diabetes-supportive diet may be challenging if you lack access to healthy foods. Some areas don't have stores that sell affordable healthy food. These areas are sometimes referred to as "food deserts."
Living in a food desert is one of the social determinants of health (SDOH) defined by the federal government. (Other examples include racism, lack of transportation, lack of safe space for exercise, low income, and polluted air and water.) Some public and private health organizations are working to address SDOH. If a SDOH is affecting your ability to manage your diabetes, talk with your health care professional. They may know of local resources that can be helpful.
Meal planning for diabetes may sound complicated at first, but your diabetes care team will help you with it. They understand that there can be a learning curve in figuring out how to eat a diabetes-supporting meal plan. You can get up to speed on healthy eating by following up with your health care professional on learning about meal planning. Be sure to let them know if you have questions or need extra help.
Move Your Body
Being active is one of the best things you can do for your diabetes health and overall health. Moving your body regularly assists not only with blood sugar control but also with managing your weight. It can also help you delay or prevent diabetes-related complications as well as many other health problems and chronic medical conditions, such as high blood pressure and unhealthy cholesterol levels.
Here's the good news: You don't have to run marathons or spend hours a day in the gym to benefit from physical activity. Just taking a daily walk can make a difference. Health experts recommend aiming for 30-60 minutes a day of moderate-intensity activity most days of the week. But if you are not physically active, don't let those lofty goals scare you off. Any activity is better than no activity. And even if you feel tired after just a couple of minutes of slow strolling, your stamina will increase over time. What feels difficult today may feel easy in a few weeks. Each day is an opportunity to challenge yourself and increase your physical strength and stamina by committing to small consistent behaviors that you can work into your daily routine.
Before you lace up your sneakers and hit the pavement, the basketball court, or the fitness center, here are a few tips to keep in mind:
- Check with your health care professional to see if exercise is safe. You may need to have cardiac or other types of testing before engaging in physical activity.
- Check your blood sugar before you exercise. If it's too high, exercise may not be safe. If it's too low, you may need to eat a snack or meal first. Using a CGM will allow you to keep an eye on your blood sugar while you are active.
- Most exercises lower blood sugar. That's good, right? It is, but it means you should track your blood sugar during and after exercise to make sure it doesn't drop too low. Your diabetes care team can let you know what to do if you experience low blood sugar.
- Stay hydrated. Drink water before and during exercise. Avoid sugary sports drinks — unless you are having a low blood sugar event.
- Your insulin may need adjusting. Insulin needs may change as you add more activity into your life. Your diabetes care team can help you understand your insulin needs.
- Protect your feet from fitness-related injuries. Wear proper-fitting socks and shoes to guard against blisters, sores, and other wounds. If you develop an injury, care for it as your health care professional has directed and let them know if it's not healing as it should.
- You may be able to work around your physical limitations. If other health conditions or physical impairments make it harder to be active, talk to your health care professional. Even if you can't go out for daily walks, other kinds of activities may help you reach your exercise goals. For example, people who have trouble walking may be able to swim, do seated fitness classes, or ride a stationary cycle. Community-based facilities such as your local YMCA may offer fitness programs for people with physical limitations.
As with healthy eating and some other diabetes-supportive behaviors, SDOH may make it harder for you to be as active as you and your diabetes care team would like. For example, you may find it difficult to move your body if your neighborhood is unsafe or you lack access to parks and other recreational resources. If a SDOH is affecting your ability to exercise, share your concerns with your health care professional. They may know of local resources that can be helpful.
Manage Your Weight
If you are overweight or have obesity, losing weight could benefit your diabetes and your overall health. (Note: If you are pregnant, talk with your obstetrician about recommended weight targets, and don't try to lose weight unless they tell you to.)
Losing weight can provide benefits to people with diabetes who are overweight or have obesity, such as:
- Lower blood sugar
- Lower hemoglobin A1C
- Less resistance to insulin, the hormone that helps blood sugar enter your cells
- Less need for diabetes medication (or lower doses of medication)
- Lower risk of diabetes-related complications
- An improved feeling of wellness
- More energy to be active and take care of your health
In addition to helping with your diabetes, losing weight if you are overweight or have obesity can reduce the progression of other health conditions, including high blood pressure, high cholesterol, heart disease, stroke, and some kinds of cancer.
Fortunately, you don't necessarily have to lose a lot of weight to realize benefits. Even modest weight loss, of approximately 5-7% of your original body weight, can lead to lower blood sugar and lower hemoglobin A1C levels.
Your health care professional can recommend a weight target that is right for you. They can also share suggestions on the type of eating plan, activities, or treatments that could help you lose weight.
You can also talk with your health care professional about whether treatment options such as weight-management medication or obesity surgery might be right for you. Learn more about obesity management and treatment in the AACE Journey for Patients With Obesity.
Did You Know?
Prediabetes
- Type 2 diabetes (T2D) can develop without warning. However, most people have prediabetes for several years before developing T2D. Fortunately, if you have prediabetes, you may be able to prevent or delay T2D with physical activity and changing your diet so you can lose weight.
- Studies have found that people with prediabetes who lost 5-7% of their body weight and added 150 minutes of exercise per week lowered their risk of developing T2D by 58-71%.
 Management of Other Health Conditions
Management of Other Health Conditions
Having diabetes can increase your chances of developing certain other health conditions. Here are some ways to lower this risk:
- Take medication for high blood pressure/high cholesterol as recommended.
- Eat a heart-healthy diet to help manage blood pressure and cholesterol.
- Monitor your high blood pressure if your health care professional recommends it and let them know if it increases.
- Keep all your appointments with your primary care provider, diabetes care team, and any specialists you see.
- Use an online scheduler, calendar, or planner to keep track of appointments.
- Tell your health care professionals if you notice any new symptoms.
- Have all of your health care professionals share test results with your diabetes care team.
- Before you leave any medical visit, ask when you should be seen again, and remember to book your next visit.
- Keep a running list of questions for your diabetes care team between appointments. Whenever you think of something, jot it down so you won't forget.
If you receive a diagnosis or treatment from your primary care provider or other health care professional, make sure they know you have diabetes. And let your diabetes care team know about care you receive from other health care professionals. In some cases, your diabetes treatment may need to be adjusted when you receive other types of medication or treatment. Similarly, your diabetes could affect other treatments you receive.
 Changes in Health Conditions or Lifestyle
Changes in Health Conditions or Lifestyle
Take Change in Stride
Diabetes is a chronic disease, meaning you will have it for the rest of your life. As you experience various life changes, they may impact your diabetes — or vice versa.
It's important to tell your diabetes care team when you face various changes in your life. Some changes may affect your blood sugar, diet, activity levels, and other factors related to your diabetes. Your diabetes care team can help you adapt your diabetes care throughout all life changes so you can:
- Manage your condition successfully.
- Lower your risk of diabetes complications.
- Feel your best.
Changes that could affect your diabetes include:
- Age
- Changes in hormone levels
- Changes in living arrangements
- Changes in support systems
- Kidney disease
- Liver disease
- Losing or gaining weight
- Mental health conditions or treatment
- Surgeries that affect your ability to exercise, such as hip or knee replacement
See Your Health Care Professional Regularly
One of the best gifts you can give yourself as someone who lives with diabetes is to see your diabetes care team as often as recommended. Regular visits allow them to identify areas for improvement and support you on your diabetes management journey.
During follow-up visits, your health care professional will:
- Adjust medication doses or insulin schedule.
- Answer questions about meal planning or exercise.
- Ask about any new symptoms you are having.
- Ask about your overall health and any health issues you are experiencing.
- Check in with you about your blood sugar control
- Check your weight and blood pressure.
- Clearly define your personalized recommended blood sugar and hemoglobin A1C goals
- Connect you with resources that may help you in your everyday diabetes management.
- Do bloodwork to check your hemoglobin A1C, a blood test that measures the average blood sugar level over the preceding three months.
- Examine you for signs of diabetes complications.
- Perform other recommended testing.
- Refer you to a registered dietitian or MNT professional to help you with meal planning as needed.
- Talk with you about follow-up appointments you may need with other health care professionals or specialists, such as dentists, cardiologists (heart doctors), nephrologists (kidney specialists), ophthalmologists (eye doctors), podiatrists (foot doctors), etc.
- Talk with you about your existing diabetes technology devices, troubleshoot any problems you are having, and discuss any new devices that may be useful to you.
Before you leave your diabetes care appointment, be sure you know when you should come back for follow-up care. Diabetes appointments are typically scheduled every three to six months, but your health care professional may wish to see you more or less often than that.
 Restorative Sleep
Restorative Sleep
You may think of getting enough sleep as a "nice to have" rather than a "need to have." If so, think again. Believe it or not, getting enough sleep can have an important impact on your diabetes management.
How does sleep connect with diabetes? To begin with, too little sleep can make your body more resistant to insulin. Also, because of the interplay between sleep and hunger hormones, being tired can make you feel hungrier than usual. What's more, feeling exhausted can also make it harder for you to stay on top of your daily routine. You may feel less like eating healthy foods, exercising, and tracking your blood sugar.
How much sleep is enough? Most adults need seven to nine hours per night. To make sure you get the sleep you need, try these tips:
- Cut back on caffeine. It may cause wakefulness even if you consume it hours before bedtime.
- Be active during the day. It can tire you out and help you sleep. But be aware that for some people, exercising too close to bedtime can keep them awake.
- Follow a relaxing bedtime routine. A warm bath, some herbal tea, or a few minutes of meditation can help relax you before you hit the sack.
- Go light on late-day liquids. Drinking less in the evening could reduce nighttime bathroom visits.
- Keep your bedroom cool, quiet, and dark. Room-darkening shades, earplugs, or an air-conditioner or fan can help.
- Set aside your devices. Using a phone, tablet, or laptop or watching television right before bed may keep you awake.
- Stay on schedule. Go to bed and get up at the same time each day.
- Take care with alcohol. Even though it can make you sleepy, consuming alcohol can lead to low-quality sleep and long-term risks to your overall health.
- Ask for help. Talk with your health care professional if you are having trouble sleeping. Sleep disorders such as obstructive sleep apnea can improve with treatment.
 Stress Management
Stress Management
Stress is more than just an annoyance for people with diabetes. It can raise or lower blood sugar, making it harder to keep your blood sugar in range. Plus, stress can make it harder for you to stick with the healthy habits that support your diabetes management, such as exercising and getting enough sleep.
Chronic stress can also raise your risk of other health problems, such as high blood pressure, obesity, and heart disease. And for some people, long-term stress can contribute to depression, anxiety, and other mental health conditions.
Avoiding stress may not be easy, especially if you are juggling work and family responsibilities with worries about your health. Managing diabetes can be stressful, especially when you are first diagnosed or if you develop a diabetes complication.
Although you can't always avoid your stressors, you can develop coping skills to help deal with stress. Some tried-and-true coping skills include:
- Exercise
- Relaxation techniques such as meditation, mindfulness, rhythmic and deep breathing techniques, stretching, and yoga
- Listening to music
- Spending time with supportive friends and relatives
- Engaging in hobbies and activities you enjoy
Speak to your health care professional if stress, anxiety, or feelings of depression are interfering with your enjoyment of life or ability to manage diabetes. They may refer you to a counselor, therapist, or stress reduction program that can help you feel better.
Thank You



 DOWNLOAD
DOWNLOAD