Diabetes Technology Glossary
A
Automated insulin delivery system: A device that combines a continuous glucose monitor (CGM) and a device that delivers insulin automatically. These systems calculate and track insulin delivery and can adjust insulin doses to help you meet your blood sugar targets.
B
Blood glucose meters: Devices that provide a snapshot of your blood sugar values at a given moment.
Blood sugar (glucose): The main energy source used by your body. After you eat food, your body breaks it down into glucose and releases it into your bloodstream, where insulin from your pancreas moves it into your cells. Although your body gets most of its glucose from carbohydrates in food, glucose can also be made from protein and fat. People with diabetes have higher-than-normal levels of glucose in their blood.
Blood sugar target ranges: Recommended target measurements for your blood sugar. Your target range is the blood sugar level your health care professional believes is best for you. Keeping your blood sugar in the recommended target range as much as possible helps you lower your risk of developing diabetes-related complications.
Bolus: A single dose of insulin taken to manage a rise in blood sugar, usually at mealtime.
C
Carbohydrate counting: A diabetes-friendly diet usually focuses on limiting how many grams of carbohydrates (starches) you eat at each meal and eating about the same number of carbohydrates at each meal. Carbohydrate counting is a process of counting and tracking the carbohydrates you eat throughout the day.
Cell replacement therapy: Therapy approved by the U.S. Food and Drug Administration in 2023 to treat people with type 1 diabetes. The therapy involves the transplantation of islet cells from a donor.
Continuous glucose monitor: Measures the glucose level in the fatty tissue of your body (interstitial glucose). Most personal CGM devices check your interstitial glucose every one to five minutes and allow you to see your glucose trends in real time and continuously. (Note: Although they may be referred to as blood sugar monitors, CGMs actually measure the glucose in the fatty tissue in your body, rather than your blood.)
D
Diabetes complications: When blood sugar is too high over a long period of time in people with diabetes, it can lead to complications (health problems) such as nerve damage, kidney damage, heart attacks, strokes, peripheral vascular disease (causing leg pain and ulcers in the feet), cataracts, and loss of vision, among others.
Diabetes smartphone apps: Applications that can support various aspects of your diabetes self-care, including education, lifestyle changes, meal planning, and medication adjustments.
Diabetes support specialists: Health care professionals who provide medical care and support for conditions that may be caused by or worsened by diabetes. These may include cardiologists (heart doctors), nephrologists (kidney specialists), ophthalmologists (eye doctors), and podiatrists (foot doctors).
Diabetes technology: Refers to any tool, device, or technology that can help you monitor your blood sugar (glucose) levels, recognize blood sugar trends, or guide you in your lifestyle choices. In addition, diabetes devices can guide you in making informed decisions about your medication doses, particularly if you use insulin therapy to manage your diabetes.
Diabetes types: There are multiple types of diabetes. The main types are type 1 diabetes, type 2 diabetes, Latent Autoimmune Diabetes in Adults (LADA), and gestational diabetes. Each type of diabetes has different causes, potential impacts on the body, and distinct risk factors. What they have in common is an inability to control blood sugar levels.
Diabetes: A condition in which your body either does not produce enough insulin or is not able to use insulin effectively. As a result, blood sugar is consistently too high, which can damage body organs and tissue. Also known as diabetes mellitus.
E
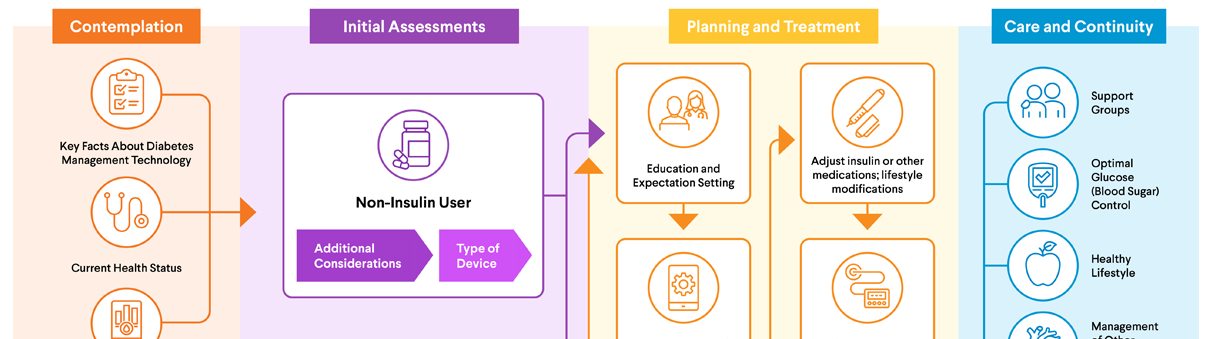
Endocrinologist: Specially trained doctor that is qualified to diagnose and treat diabetes and hormone-related diseases and conditions. This AACE tool can help you find an endocrinologist near you.
F
Fasting blood glucose test: A test used to diagnose diabetes. For this test, a person is asked not to eat anything for at least eight hours before blood is drawn. A result of 126 mg/dl or higher typically leads a health care professional to diagnose diabetes.
G
Gestational diabetes: Diabetes that develops during pregnancy. It is usually a temporary condition that goes away after the end of pregnancy.
Glucometer: A device that measures blood sugar from a finger-prick blood sample.
Glucose, or blood glucose: Other names for blood sugar.
H
Hemoglobin A1C test: This is a blood test that shows the average blood glucose over the previous three months. A result of 6.5% or higher typically results in the diagnosis of diabetes. Also known as HbA1C test or A1C test.
Hyperglycemia: When your blood sugar gets too high. Also known as high blood sugar, this is a potentially dangerous condition that can lead to a variety of possible diabetes complications (health problems) such as nerve damage, kidney damage, heart attacks, strokes, peripheral vascular disease (causing leg pain and ulcers in the feet), cataracts, and loss of vision, among others.
Hypoglycemia: When your blood sugar gets too low. Also known as low blood sugar, this is a potentially dangerous condition in people with diabetes. Treatment involves quickly getting your blood sugar back up with high-sugar foods, drinks, or medications. Untreated hypoglycemia can lead to seizures, loss of consciousness, and in severe cases, death.
I
Inhaled insulin: Powdered insulin that you can inhale for bolus (mealtime) doses.
Insulin pen: A device that looks like a writing pen, but contains a needle that can inject insulin. Most pens come pre-filled with insulin. After using all the insulin in the pen, you discard the pen. With refillable pens, you insert an insulin cartridge and then replace it after use.
Insulin pump: A device that can give you insulin continuously without the need for multiple daily injections.
Insulin (hormone): A hormone produced by your pancreas gland. Insulin controls the level of glucose (a type of sugar) in your blood.
Insulin (medication): An injected (or in some cases, inhaled) medication that people with diabetes may take to help manage their blood sugar. Insulin medication mimics the action of your body's own insulin, which moves glucose (blood sugar) from your bloodstream into your cells.
Islet cells: Cells within your pancreas that produce insulin and other hormones.
L
Latent Autoimmune Diabetes in Adults (LADA): A form of diabetes that appears in adulthood, typically characterized by a slow and gradual onset. It shares features with both Type 1 and Type 2 diabetes, making it a bit of a hybrid condition. LADA develops when the body's immune system mistakenly attacks the cells in the pancreas that make insulin, a hormone that controls blood sugar.
M
Medical nutrition therapy (MNT): Nutrition care provided by a registered dietitian nutritionist. It includes education, advice, and follow-up care centered around healthy eating and behavior changes. MNT may be covered by your health insurance. Your health care professional can tell you whether MNT is right for you.
mg/dL: A unit of measure used in the U.S. to show the amount of glucose (blood sugar) in your blood. Stands for milligrams per deciliter.
O
Obesity: A biological, preventable, and treatable disease that means a person has too much body fat. There are different factors that can contribute to a person having obesity, including family history and environment. Health care professionals may use body mass index (BMI) as a way to determine whether you are obese. Someone is considered obese if their BMI is 30 or above. Also known as adiposity-based chronic disease (ABCD). Having obesity raises the risk of developing type 2 diabetes. Learn more about obesity management and treatment in the AACE Journey for Patients With Obesity.
Oral glucose tolerance test: A test used to diagnose diabetes. With this test, your fasting blood glucose is tested; then you consume a glucose-rich drink, followed by another blood sugar measurement two hours later. A result of 200 mg/dl or higher typically results in a diagnosis of diabetes.
P
Pancreas: An organ located behind your stomach that produces insulin, a hormone that moves glucose (blood sugar) from your blood to your cells.
Patch pumps: Devices that attach directly to your skin via a self-adhesive pad that houses the insulin delivery system along with a cannula (small plastic tube) or tiny needle that is inserted into the skin. Depending on the model, you control the patch pump directly via the device or using a handheld device or smartphone app. Some (but not all) patch pumps can calculate or track insulin doses.
Prediabetes: When your blood sugar is higher than it should be, but not high enough to be considered diabetes. Prediabetes often precedes the development of type 2 diabetes. With lifestyle changes such as weight loss, exercise, and changes in eating habits, type 2 diabetes may be delayed or prevented in people with prediabetes.
R
Registered dietitian: A health care professional who is an expert in food and nutrition and has met certain requirements for education and credentialing. Dietitians can play a key role in managing diabetes. They offer individualized support based on your personal lifestyle and goals while also understanding the complexities of the disease. Also known as a registered dietitian nutritionist. Visits with a registered dietitian may be covered by your health insurance.
S
Smart (connected) pen caps: Devices that attach onto the top or side of most disposable insulin pens available today. They connect wirelessly to a continuous glucose monitor and a smartphone app. The CGM system sends real-time blood sugar data to the smart pen cap. The screen on the cap, in turn, tells you how much insulin to take based on your blood sugar levels and your health care professional's recommendations. The cap also keeps track of insulin timing and dosing and reminds you if you miss a needed dose.
Smart insulin pen: A prefilled insulin pens that can connect to a smartphone app to simplify management of insulin delivery. It may be recommended if you require mealtime insulin and do not use an insulin pump.
Social determinants of health (SDOH): Factors outside your body that may affect your health, well-being, and quality of life, such as where you are born, live, learn, and work. In many lower socioeconomic communities, SDOH can raise your risk of type 2 diabetes, obesity, and other health problems.
Syringe: A needle used to inject insulin into fatty tissue just under the skin. A syringe consists of a hollow plastic tube with a needle and a plunger.
T
Time above range: The amount of time your blood sugar stays above your target range. Spending too much time above range is a sign of hyperglycemia (high blood sugar), which can create long-term complications.
Time in range (TIR): The percentage of time your blood sugar stays within your target range. Generally, health care professionals recommend aiming for a TIR of about 17 hours a day (~70% of the time). Consult with your diabetes care team to determine the best TIR for you.
Traditional insulin pumps: Devices worn on your body that deliver insulin into the fatty tissue just below the surface of your skin, where it is absorbed into your bloodstream. Advanced insulin pumps can also calculate and track insulin doses.
Type 1 diabetes: Develops when the cells that produce insulin in your pancreas are mistakenly destroyed by your own immune system. Your body is unable to produce enough insulin, which means that blood sugar is not controlled and can become very high. Previously also known as juvenile diabetes or insulin-dependent diabetes.
Type 2 diabetes: Occurs when cells become resistant to the effects of insulin, which results in uncontrolled blood sugar. May develop in adults, teens, or children. Obesity is a significant risk factor for type 2 diabetes. Previously also known as adult-onset diabetes or non-insulin- dependent diabetes.



 DOWNLOAD
DOWNLOAD