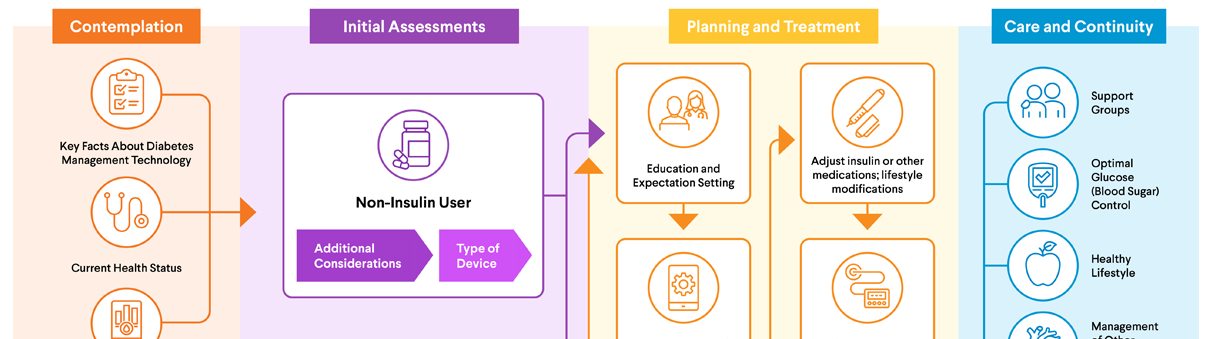
Initial Assessments
Planning & Treatment

Planning & Treatment
Education and Expectation Setting
The idea of managing your diabetes can seem overwhelming. How will you check your blood sugar (glucose) levels? What's the best way to take the insulin your body needs? How can you make sure you don't miss any doses?
There's a lot to consider. But the good news is that you won't be on your own. Your diabetes care team will be there to educate you, help set up a testing schedule, let you know a target range for your blood sugar numbers, and more.
If you have type 1 diabetes: You will need to inject insulin using a syringe/needle, pen, or insulin pump. The best way to do this will depend on your personal preferences and input from your diabetes care team.
If you have type 2 diabetes: While some of the most important treatments are lifestyle changes, non-insulin diabetes medications are often prescribed. Insulin may be added later.
 Device Setup and Consultation
Device Setup and Consultation
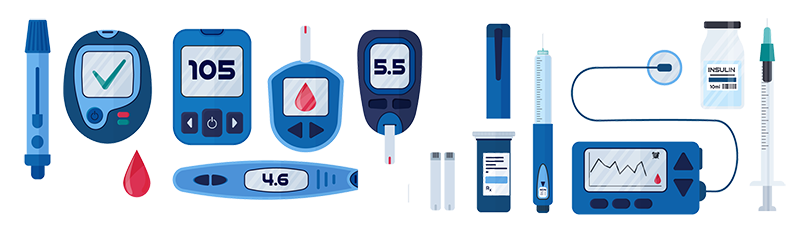
Before beginning to use new diabetes technology, your care team will review the types of devices, basic functions, and other key information that will help you get the most out of the device. Managing your diabetes involves using two basic types of devices: glucose monitors and insulin delivery devices. Both come in a variety of models that vary in terms of features, cost (and whether they are covered by insurance), ease of use, and other factors. Be sure to consult your health care professional and insurance company to learn which options may be available for you, and visit our AACE Prescription Affordability Resource Center for affordability assistance.
Glucose Monitors
Having diabetes means you must always be aware of your blood sugar levels.
For most people, blood sugar rises and falls within a small range throughout the day. In people with diabetes, the range can be much wider. You have to strike the right balance between treating hyperglycemia (high blood sugar) and avoiding hypoglycemia (low blood sugar).
There are two basic options for monitoring your blood sugar: blood glucose meters and continuous glucose monitors. Read on to learn which might be right for you.
Continuous Glucose Monitors
A continuous glucose monitor (CGM) enables you to monitor your blood sugar 24 hours a day. CGM systems may consist of two or three parts:
- Sensor: A tiny sensor inserted under the skin measures your blood sugar every few minutes. Depending on the model, your age, and the manufacturer's recommendations, you will wear the sensor on the back of an arm, the abdomen, or another location. Also, depending on the model, the sensor must be replaced every seven to 180 days.
- Transmitter: Some sensors may need to be connected to a small transmitter to allow the CGM to send glucose readings wirelessly to a receiver or reader.
- Receiver or reader: This is a rechargeable standalone device or an app on a smartphone or tablet. It receives blood sugar data from the transmitter or the sensor directly. It then displays current blood sugar levels, historical trends in levels, and arrows showing the direction that blood sugar is heading.
A CGM system collects data that shows how often your blood sugar is above or below your target range, possible areas for improvement, and more. You and your diabetes care team can use this information to make decisions about your diabetes care plan. For example, you may need to make changes to your diet or find ways to address low blood sugar events.
Your health care professional may recommend a CGM if:
- You require insulin injections or use an insulin pump.
- You have frequent episodes of low blood sugar.
- Your blood sugar levels tend to vary a lot.
- You are pregnant and have diabetes.
CGM systems measure blood sugar concentrations in body fluid, which reflect blood sugar levels. In contrast, blood glucose meters measure glucose levels directly in the blood. Why is this important? Measurements from a CGM can lag several minutes behind those from a blood glucose meter — especially when blood sugar levels are changing rapidly, such as after a meal.
FDA Early Alert: FreeStyle Libre 3 and FreeStyle Libre 3 Plus CGM Sensor Issue
The FDA has issued an Early Alert for select FreeStyle Libre 3 and FreeStyle Libre 3 Plus CGM sensors due to reports of falsely low glucose readings that may affect treatment decisions. This alert does not apply to the Libre 3 app, reader, or other Libre products. Read the full FDA alert here.
CGM Device Comparison
Compare and contrast FDA-approved CGM systems.
View Comparison Chart
Having a backup plan
CGMs are incredibly valuable in managing diabetes. So what happens if yours malfunctions or has a dead battery? What if it stops working due to a power or internet outage? What if it gets damaged? What if you run out of supplies before your insurance approves you to pick up new ones?
Situations like these are why it's important to have a backup plan. Be sure to talk this over with your diabetes care team. For starters, consider having a spare CGM system (even an older model will do in a pinch) along with a blood glucose meter and test strips.
Having a non-working CGM on your hands is never ideal. But with a good plan, you'll have peace of mind knowing you can get by until the CGM is working again or replaced.
Blood Glucose Meters
Blood glucose meters require you to draw a small amount of blood, typically from your fingertip. First, you place the test strip in the meter. Next, you use a special needle (lancet) to prick the skin and then squeeze a blood droplet onto a test strip.
After a few seconds, the blood glucose meter displays your blood sugar level on the screen. This is a snapshot of glucose values at a given moment.
It's important to track your results. You can choose from many smartphone apps or keep a written daily record for this purpose. Many meters can also be downloaded in the clinic. Having this data is useful when meeting with your diabetes care team.
Insulin Delivery Devices
Select any of the insulin delivery devices listed below to navigate directly to that section.
- Syringes
- Insulin Pens
- Smart (Connected) Insulin Pens
- Smart (Connected) Pen Caps
- Traditional Insulin Pumps
- Patch Pumps
- Automated Insulin Delivery
- Inhaled Insulin
The most common way to take insulin is an injection into fatty tissue just under the skin. Options for insulin injection include syringes, insulin pens, and insulin pumps.
Syringes
A syringe consists of a hollow plastic tube with a needle and a plunger. After drawing the correct amount of insulin from a vial, you insert the needle into your skin. Then you push the plunger to inject the insulin.
Insulin Pens
An insulin pen looks like a writing pen, but a needle is connected to one end to inject the insulin. Most pens come pre-filled with insulin. After using all the insulin in the pen, you discard the pen. With refillable pens, you insert an insulin cartridge and then replace it after use.
Smart (Connected) Insulin Pens
The smart insulin pen is a newer option for insulin delivery. It may be recommended if you require bolus (mealtime) insulin and don't use an insulin pump.
A smart insulin pen connects wirelessly to a smartphone app and a CGM to simplify management of insulin delivery. This system automatically performs functions like these:
- Tracking insulin dosing (such as when insulin was administered and how much was given)
- Calculating insulin doses
- Providing downloadable data reports
- Sending "missed dose" reminders
- Transmitting data to your health care team
Smart (Connected) Pen Caps
Smart pen caps attach onto the top or side of most disposable insulin pens available today. They connect wirelessly to a continuous glucose monitor and a smartphone app.
The CGM system sends real-time blood sugar data to the smart pen cap. The screen on the cap, in turn, tells you how much insulin to take based on your blood sugar levels and your health care professional's recommendations. The cap also keeps track of insulin timing and dosing and reminds you if you miss a needed dose.
The smart pen cap can send information about insulin timing and dosing to a smartphone app or cloud-based data portal. That allows you and your diabetes care team to monitor your progress over time.
Traditional Insulin Pumps
An insulin pump is a small device that delivers insulin to manage blood sugar. It's usually worn on a belt clip or in a pouch or pocket. Some models attach directly to the skin.
With most models, insulin from the pump passes through a skinny plastic tube inserted into fatty tissue just under the skin. The most common sites are the stomach area or back of the upper arm.
The pump delivers insulin in two ways:
- A low and constant flow to maintain blood sugar levels overnight and before meals. This is known as "basal dosing."
- Additional bursts of insulin at mealtimes. This is known as "bolus dosing."
Insulin pumps have a digital display that lets you program the amount and frequency of insulin deliveries. Many models can be controlled from smartphones. Some models have advanced features to automate insulin dosing.
Patch Pumps
For many people with diabetes, the patch pump is an appealing alternative to the traditional pump. Patch pumps attach directly to your skin via a self-adhesive pad that houses the insulin delivery system along with a cannula (small plastic tube) or tiny needle that is inserted into the skin. Depending on the model, you control the patch pump directly via the device or using a handheld device or smartphone app.
The patch pump and cannula must be changed every two to three days. You should switch sites each time to improve insulin absorption.
In addition to their smaller size, patch pumps have many advantages over traditional pumps. In one analysis, researchers found "evidence that patch pumps improve quality of life, reduce diabetes-related distress, increase patient satisfaction, and are preferred by patients compared to conventional insulin pumps and multiple daily injection therapy."
Automated Insulin Delivery
Insulin pumps can be paired with a CGM system to create an automated insulin delivery (AID) system. This option is recommended for people with type 1 diabetes or people with type 2 diabetes that require meal time insulin to reach their glucose targets.
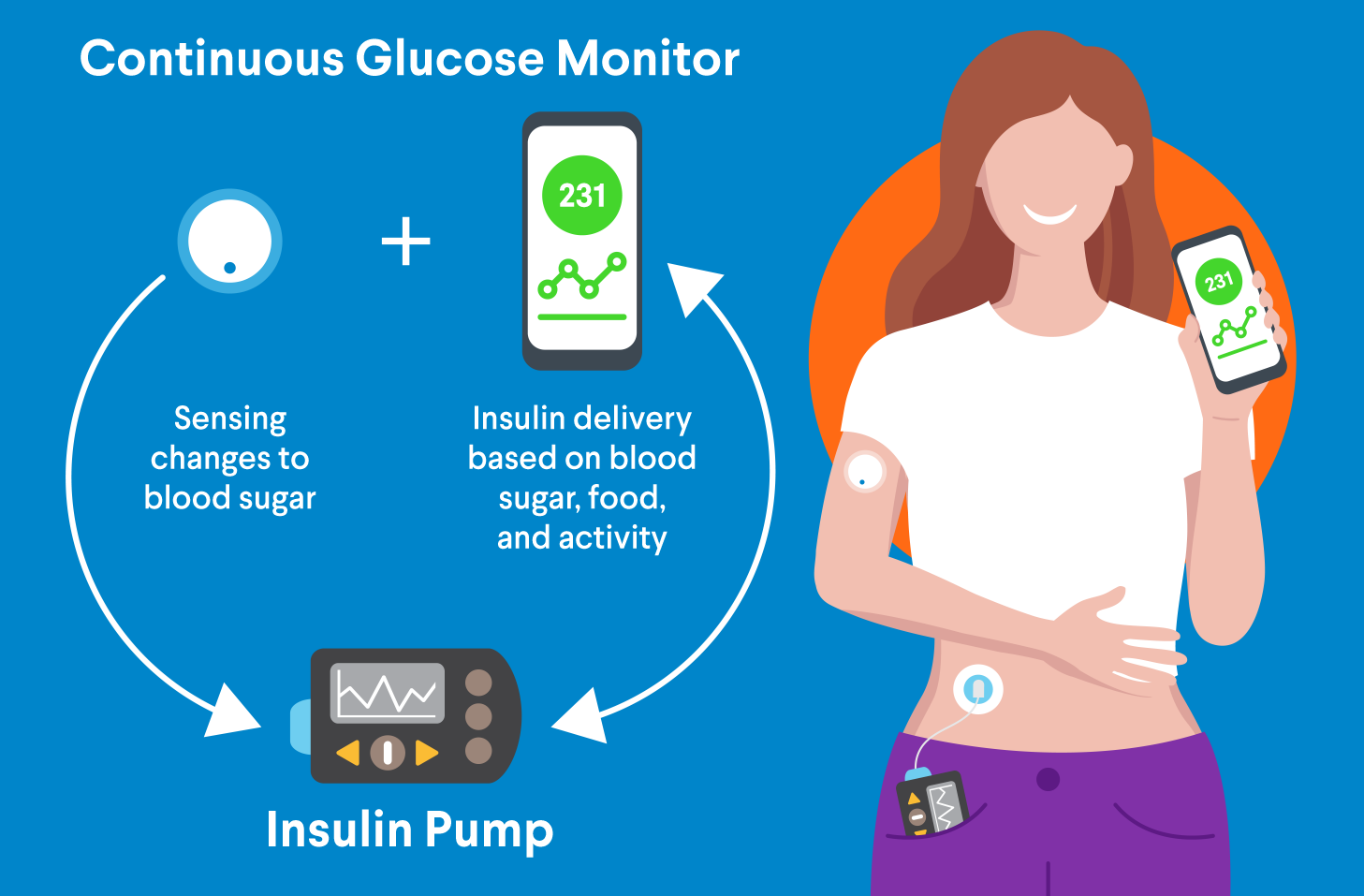
Here's a brief summary of how an AID system works:
- The CGM system measures blood sugar levels in body fluid, which reflect blood sugar levels, every few minutes. It sends the information to a software program on a smartphone app or in the insulin pump.
- The program figures out how much insulin your body needs and sends the information to the pump.
- The pump delivers small doses of insulin whenever your blood sugar is above your target range and decreases insulin delivery if your blood sugar falls below your target range.
- Before eating, you must manually enter carbohydrate contents of the meal. This allows the system to calculate and deliver the appropriate insulin dose.
With any insulin pump, it's important to keep insulin pens or vials and syringes available in case the pump stops working.
Future enhancements to AID systems are expected to further increase time in range and reduce user burden.
In addition, researchers hope to develop a fully closed-loop system, which would automatically calculate and deliver mealtime doses without the need to enter carbohydrates or announce meals. Also under development: a dual-hormone (insulin and glucagon) closed-loop system.
Inhaled Insulin
Want to rely less on injections to take your insulin? Inhaled insulin may be an option for your bolus (mealtime) doses.
Here's how it works: Before each meal, you use an inhaler device to breathe powdered insulin into your mouth. The insulin quickly passes into your lungs and then your blood.
For your basal (long-lasting) doses, you will still need to use injections or a pump.
Devices for Measuring Ketones
If your blood sugar is 240 mg/dL or higher, use an over-the-counter test kit to check for ketones every four to six hours. Three common options are urine, blood, and breath ketone tests.
Based on test results, you may need to seek immediate emergency care. Or your health care professional may adjust your insulin dosage or recommend other changes to lower your ketones.
Urine Ketone Tests: Urine ketone tests are designed to detect high ketone levels in the urine. At-home test kits are inexpensive and available at most pharmacies. A prescription is not required.
With most urine ketone tests, you collect a small urine sample in a container. Next, you dip a test strip in the urine sample. A change of color means ketones are present. The number of ketones is typically labeled as "small," "moderate," or "large."
Be sure to carefully review the instructions prior to using a urine ketone test. If you have any questions, contact your health care professional.
Blood Ketone Tests: Blood ketone tests are designed to detect high ketone levels in the blood. They are more accurate and deliver results faster than urine ketone tests. This is critical because receiving timely care is essential if you have high ketones.
At-home blood ketone tests involve pricking your finger to collect a blood sample. You place a drop of blood on a test strip, which is inserted in a blood ketone meter. The meter tells you the concentration of ketones in your blood. A higher concentration indicates a greater risk of DKA.
Some blood glucose meters check both blood glucose and ketone levels.
Breath Ketone Tests: Handheld breathalyzers are designed to detect acetone, a type of ketone. However, they are not recommended for ketone tests in people who may have DKA, as the technology is unproven.
Ketone Monitoring Systems
Ketone monitoring systems are more complex than ketone blood meters. They can provide real-time ketone readings and monitor blood sugar levels as well. A number of ketone monitoring systems are available today. Ask your health care professional if one might be right for you.
Cell Replacement Therapies
In 2023, the U.S. Food and Drug Administration approved the first cell replacement therapy to treat people with type 1 diabetes. The therapy involves the transplantation of islet cells from a donor. After one or two infusions, some patients will no longer need to take insulin to control their blood sugar levels because the transplanted islet cells will produce enough insulin on their own. Please note: This therapy is only for people experiencing significant hypoglycemia (low blood sugar) and requires lifelong immunosuppressant therapy.
Another cell replacement therapy that is in early development may provide another treatment option for people with type 1 diabetes. This technology would allow for a transfusion of laboratory-grown insulin-producing cells to replace damaged or missing islet cells.
 Reevaluation and Adjustments
Reevaluation and Adjustments
Once you have started using a device, your care team will work with you to reevaluate how well your diabetes is controlled by looking at factors including time in range, A1c, and your quality of life. Adjustments may be necessary for your lifestyle, the amount or type of insulin you are taking, or other medications you are taking. All of these adjustments will help you manage your diabetes.
 Changing to a Different Device
Changing to a Different Device
Each year, you and someone from your diabetes care team should discuss the diabetes technology you have been using. Consider questions like these:
- Are all your devices working as you would like them to?
- Do any of your devices lack features you need or would like to have?
- Are any of your devices nearing the end of their life and in need of an update?
- Have there been any changes to your health that would mean you could benefit from a different device?
- Would any new technologies be better for you than your current device?
- Are you interested in learning about new devices as they become available?
Also, has your health insurance changed in terms of which devices it covers? If so, do you have coverage for different devices than your insurance would cover last year? (Always keep in mind that cost and insurance coverage may impact some decisions about devices.) Visit our AACE Prescription Affordability Resource Center for affordability assistance.
What to Know About Long-Term Use of Devices
Here are a few important points to keep in mind:
- Follow manufacturer instructions for cleaning devices and stick to the recommended schedule.
- Work with your diabetes care team to ensure your alerts are always set to meet your needs
- To reduce the risk of infection or irritation, prepare your skin properly before applying a sensor, inserting an infusion set for an insulin pump, or giving an insulin injection.
- Remove sensors gently to avoid harming your skin.
- Rotate the placement of sensors or needle sticks to avoid scarring.
- Always keep up with the latest app updates and integrations.
- Keep usernames and passwords in a secure location that you won't lose.
Key Terms You Should Know
Time in Range
Time in range (TIR) is the percentage of time your blood sugar stays within your target range. This target range is typically a blood sugar level between 70 and 180 mg/dl for non-pregnant people. Most people with diabetes aim for a TIR of about 17 hours a day (~70% of the time).
Your personal blood sugar target depends on factors such as your age and overall health. For example, a TIR of around 50% of the day may be recommended if you have other medical conditions that low blood sugar can affect. A CGM will help you track your blood sugar levels all day long.
Your health care professional will offer guidance on how to stay within your range. For example, this may involve adjusting your medication and/or insulin, changing your diet, or increasing your activity.
Time Below Range
For most people, the low end of their target range is 70 mg/dL. Spending too much time below range is a sign of hypoglycemia (low blood sugar). Your diabetes care team can help you take steps to avoid and manage this potentially dangerous condition. They may also recommend that you carry emergency glucagon to use if you experience severely low blood sugar (below 54 mg/dL).
Time Above Range
For most people, the high end of their target range is 180 mg/dL. Spending too much time above range is a sign of hyperglycemia (high blood sugar), which can create long-term complications. Your diabetes care team can help you reduce instances of and manage this condition.
A1c Test
The A1c test (also known as the hemoglobin A1c test or the HbA1c test) is a blood test that shows your average blood sugar over the previous three months. It is one of the ways that diabetes is diagnosed. Your diabetes care team will also do A1c tests to check how well your care plan is working.
A high A1c number means too much sugar is in your blood because your body isn't absorbing it.
| A1c Number | Result |
|---|---|
| 5.6% or below | Normal (no diabetes) |
| 5.7% to 6.4% | Prediabetes |
| 6.5% or higher | Diabetes |
Following a diagnosis, your diabetes care team will give you an A1c test about every three to six months. Normal A1c levels are 5.6% or below. Most people with diabetes should aim for less than 6.5%, though this number varies from person to person. If you have prediabetes, an A1c level that nears 6.4% will increase your risk of developing type 2 diabetes.
Keep in mind that A1c tests don't replace daily blood sugar checks throughout the day.
TIR vs. A1c
Remember: An A1c test shows your average blood sugar over the previous three months. For many years, health care professionals relied mainly on this number to assess a patient's overall blood sugar control.
The emergence of CGMs around 1999 changed the picture. By checking time in range, these devices offer a much more accurate measure of your blood sugar control on a day-to-day basis.
For example, suppose your blood sugar varies wildly from low to high throughout the day. Since A1c is a snapshot of your average blood sugar over the previous three months, it won't capture those variations. Your A1c number could be fine but hide an underlying problem.
On the other hand, TIR will let you know if you are experiencing low and/or high blood sugar at all times of day or night. As a result, you and your diabetes care team can work on avoiding those fluctuations (and the resulting complications).
Setting Alerts and Reminders
CGMs can be programmed to alert you when your blood sugar is:
- Too low
- Too high
- Falling or rising too quickly
Setting your CGM requires you to enter your target ranges and other information. Ask your diabetes care team if you need any help.
CGMs also allow you to set reminders for things like taking your bolus (mealtime) dose or checking your blood sugar at certain times of the day.
Sharing Your Data With Others
CGMs let you share your data and alerts with others, typically via a smartphone app.
Giving family members and friends access to this information is a matter of safety. For example, suppose you are sleeping alone in a hotel room and a low glucose alert fails to wake you up. In that case, someone else will receive the notification and try to offer assistance.
You can also share data with health care professionals. This can help you stay within your target blood sugar range. In addition, it helps you and your diabetes care team make informed decisions about your insulin dosing and timing along with other aspects of your care plan.
 Maintenance
Maintenance
Maintaining your diabetes technology is crucial for ensuring its accuracy and reliability in managing your condition. Regularly check and clean your devices, such as glucose meters, insulin pumps, and CGMs, according to the manufacturer's instructions. Always have a backup plan, including spare batteries, emergency contact numbers, and manual methods to monitor and manage your diabetes in case of technology failure. By taking these steps, you can maintain the effectiveness of your diabetes technology and continue to manage your diabetes confidently.



 DOWNLOAD
DOWNLOAD