Hyperthyroidism and Graves' Disease Treatment
Hyperthyroidism and Graves' Disease Treatment
How is hyperthyroidism treated?
Hyperthyroidism treatment will depend on your age, health, case, and the severity of your condition. Speak with your health care professional to determine the best treatment plan for your personal condition.
Common treatment options for hyperthyroidism include:
- Anti-thyroid medications: Two drugs are available for treating hyperthyroidism: propylthiouracil (PTU) and methimazole (Tapazole). Methimazole is usually preferred because PTU can rarely cause severe and potentially fatal liver damage. These medications control hyperthyroidism by slowing thyroid hormone production. They may take several months to normalize thyroid hormone levels.
- Some patients experience a remission of hyperthyroidism after treatment with these drugs, but the remission is sometimes only temporary.
- Anti-thyroid drugs may cause an allergic reaction, such as a rash or hives, in about 5% of patients who use them. Also, in rare cases, the drugs may cause a dangerously lower white blood cell count, which will increase susceptibility to infection.
- Radioactive iodine treatment: Radioactive iodine is usually taken orally. It enters the thyroid cells from the bloodstream and gradually destroys them. Results are usually seen in 8 to 12 weeks, although it can take up to six months.
- If too low of a dose of radioactive iodine is given and enough cells are left alive, hyperthyroidism almost always recurs. Therefore, most endocrinologists strive to destroy the diseased thyroid gland with a single dose of radioiodine.
- This results in the intentional development of an underactive thyroid (hypothyroidism), which is easily treated with lifelong thyroid hormone replacement therapy.
- Surgical removal of the thyroid: In rare circumstances, operating to remove most of the thyroid gland is recommended. For example, surgery may be the best option for a pregnant woman with a severe uncontrolled disease in whom radioiodine would not be safe for the baby, or in patients who have large nodules causing symptoms
- Surgery usually leads to hypothyroidism, which is treated by lifelong thyroid hormone replacement therapy.
- Other treatments: Beta blockers may be used temporarily to control hyperthyroid symptoms until other therapies take effect. In cases where hyperthyroidism is caused by thyroiditis or excessive ingestion of either iodine or thyroid hormone, time or an adjustment of iodine or thyroid hormone dosing may be the only type of treatment required.
- Additionally, iodine drops are prescribed when hyperthyroidism is severe or sometimes prior to undergoing surgery for Graves' disease.
Graves' Disease Treatment Options
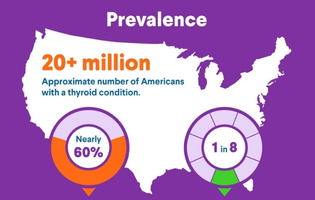
Graves' disease is the most common cause of hyperthyroidism.
Treatment for Graves' disease can include one or more of the following:
- Radioactive iodine therapy: Radioactive iodine is a capsule or liquid that destroys the overactive thyroid cells over time.
- Anti-thyroid medications: Used to slow down how much thyroid hormones your body makes. Anti-thyroid medications are currently the most common treatment option.
- Beta blockers: These medications help block the effects of hormones on the body and are especially helpful in the beginning when waiting for other treatments to take effect.
- Surgery: Surgery usually takes the form of thyroidectomy (complete removal of the thyroid gland). After surgery, medications can be taken to supply the body with normal amounts of thyroid hormone.
Don't ignore shaky hands and a rapid heartbeat. Contact your health care professional if you are experiencing any common symptoms related to Graves' disease.
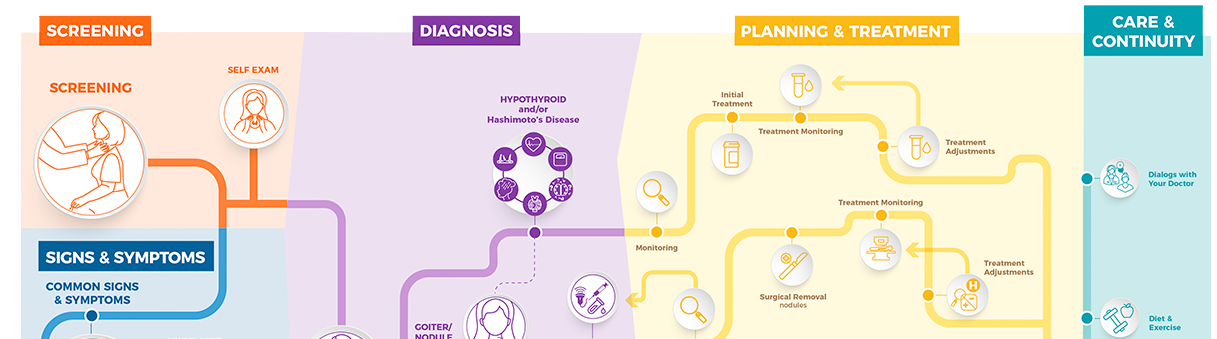
 Treatment Monitoring
Treatment Monitoring
How is hyperthyroidism treatment monitored?
After you receive treatment for hypothyroidism, your health care professional will monitor you to make sure the treatment worked as planned and to ensure that your thyroid hormone levels reach and remain in the normal range. It's important that your thyroid hormone levels aren't too high or too low, because having too much or too little thyroid hormone can negatively affect how your body functions.
To check on your thyroid after hyperthyroidism treatment, your health care professional will likely schedule tests that measure the TSH, T4, and/or T3 in your blood. Low TSH and high T3 and T4 may suggest your thyroid is still overactive. High TSH and low T3 and T4 may suggest that your thyroid is not active enough and that it has gone from being overactive to underactive (hypothyroid).
If monitoring shows that you still have hyperthyroidism after receiving treatment, your health care professional may recommend increasing the dose of your anti-thyroid drugs or further treatment with radioactive iodine or surgery. However, if monitoring shows that hyperthyroidism treatment has caused your thyroid to become underactive — which often happens after hyperthyroidism treatment — they will likely prescribe thyroid hormone therapy to replace the hormones your thyroid is no longer making. This treatment generally consists of taking a single daily tablet of a medication known as levothyroxine.
If you take levothyroxine, keep in mind that different people need different amounts of this medication. Determining your own personal just-right daily dose often requires monitoring and adjustment by your health care professional.
Your health care professional monitors your levothyroxine treatment by performing blood tests to measure the amount of TSH and T4 in your blood. Generally, recommend blood tests about six to eight weeks after you begin taking levothyroxine. If your health care professional needs to adjust your dose, they typically recommend another round of blood testing six to eight weeks later. Don't be surprised if you need several dose adjustments to get to the right levothyroxine dose — that's not unusual.
Once your health care professional settles on a levothyroxine dose that brings your TSH and T4 into the normal range, they will likely recommend follow-up blood testing every six to 12 months to make sure your dosage stays on track long-term. Levothyroxine dose adjustments may become necessary because of changes in your thyroid function or because of factors such as weight loss or gain, other medicines you take, or changes in your health.
Although blood tests can determine whether your thyroid hormone level is within normal range, symptoms can also indicate whether your treatment needs adjusting. Beta blockers are often used to help control symptoms of hyperthyroidism while treatment is taking effect, and their dose may need to be adjusted if symptoms are not improving. Let your health care professional know if you start or continue experiencing any of the following:
- Bowel movement changes (diarrhea or constipation)
- Changes in energy levels, sleep habits, or tiredness
- Changes in heart rate, including a pounding heart
- Feeling unusually cold or warm
- Feelings of depression, anxiety, or irritability
- Menstrual changes
- Muscle aches or weakness
- Nervousness, jumpiness, or shakiness
- Problems getting pregnant
- Unexplained weight changes
 Treatment Adjustment
Treatment Adjustment
Why does hyperthyroidism treatment need to be adjusted?
Depending on the type of hyperthyroidism treatment you receive, you may require adjustments to your treatment.
- Anti-thyroid medications: Propylthiouracil (PTU) and methimazole (Tapazole) gradually reduce your hyperthyroidism symptoms by limiting your thyroid's ability to produce hormones. Patients typically stay on these drugs for a year or longer as stopping early markedly increases the risk of recurrence of hyperthyroidism. If you take one of these medications, your health care professional will monitor your thyroid hormone levels with blood tests and will take you off your medication if you appear to be in remission.
- Your health care professional may also take you off medication if you experience an allergic reaction or liver damage. If you develop an underactive thyroid, your health care professional will usually lower your dose. If the underactive thyroid persists, your health care professional will prescribe thyroid hormone replacement therapy (levothyroxine), which you take for the rest of your life. Be sure to let your health care professional know if you develop yellowing of your skin or eyes (jaundice), fever, loss of appetite, or abdominal pain.
- Radioactive iodine treatment: This treatment causes your thyroid to shrink, usually within three to six months. If you receive this treatment, your health care professional monitors your thyroid hormone levels with blood tests and takes you off it when you no longer need it. The standard of care is to try to destroy the diseased thyroid gland with a single dose of radioiodine. You may develop an underactive thyroid as a result of this treatment. Your health care professional will prescribe thyroid hormone replacement therapy (levothyroxine), which you take for the rest of your life.
- Surgical removal of the thyroid: hyperthyroidism surgery, which removes most of your thyroid gland, typically leads to hypothyroidism, which is treated with lifelong thyroid hormone replacement therapy.
- Dietary changes: Your health care professional may recommend that you limit your intake of iodine in foods, supplements, and medications such as cough syrups, because iodine can worsen hyperthyroidism, depending on the underlying cause. In some cases, iodine will help treat Graves' disease, but it will make toxic nodular goiter worse. Foods that contain significant amounts of iodine include seaweed such as kelp, nori, kombu, and wakame. Other sources of iodine include seafood and commercially manufactured bread made with iodine-based dough conditioners.



 DOWNLOAD
DOWNLOAD