Home
Contemplation
Contemplation
If you have obesity, you've probably wondered at some point why you gained your extra weight. And you've likely received a lot of unwanted input about this. Perhaps people have told you it's because you eat too much or don't exercise enough. They may even have blamed your obesity on a lack of willpower or an unwillingness to try hard enough to shed excess pounds.
While it's true that food, activity, and effort play a role in obesity, there's much more to it than that. Scientists now know that obesity is a very complex condition that goes way beyond calories and willpower. Obesity is not a character flaw — it's a chronic disease.
Obesity has a long list of potential causes, ranging from the genes you were born with to the environment in which you live. Everyone's body is different, and everyone has an individual susceptibility to obesity.
Here are some of the factors that can increase your risk of developing obesity:
- The food you eat: Excess weight gain is likely to occur when you regularly eat more calories than you burn each day.
- Your activity levels: All the activity you do, from workouts at the gym to walking your dog, burns energy from the foods you eat. Being less active burns less energy.
- Your genetics: Your genes can affect how much body fat you store, how you process it, and where the fat goes. They can also affect your appetite. If your family members have obesity, there's a greater chance that you'll develop the disease, too.
- Your upbringing: You may have picked up obesity-influencing eating and activity habits in the home where you were raised.
- Your race or ethnicity: Certain demographic groups are more likely than others to have obesity. For example, non-Hispanic Black adults have the highest obesity rates, followed by Hispanic adults, non-Hispanic white adults, and non-Hispanic Asian adults.
- Your environment: Many things in the world around you can influence your weight. These include where you live and whom you live with; your economic status; your education level; your job; and your access to medical care, healthy food, and a place to exercise. These conditions are referred to as social determinants of health (SDOH). They can have a major impact on your weight, health, and well-being.
- Your health: Certain medical conditions may make it easier to gain weight and harder to lose weight. These include Cushing's disease, arthritis, hypothyroidism, depression, polycystic ovary syndrome, and sleep apnea. Chronic stress and inadequate sleep are additional factors.
- Your mental health: Some kinds of mental health conditions can affect your weight. For example, if you're depressed, you may turn to food when experiencing sad feelings. In addition, you may find it difficult to motivate yourself to exercise. Chronic stress and anxiety may also affect your eating and exercise habits.
- Eating disorders and dysregulated eating: These phrases describe a range of abnormal eating behaviors, including bulimia, anorexia nervosa, binge eating, and purging. Because these behaviors can make it harder to recognize your body's hunger and fullness signals, they may lead you to overeat and gain excess weight.
- Your age: As you get older, you may gain weight or struggle to lose weight because of hormonal changes, a less active lifestyle, and/or a reduction in muscle mass.
- Your medications: Some prescription drugs are linked to weight gain.
- Your sleep habits: A lack of sleep, along with sleep disorders such as obstructive sleep apnea and shift work sleep disorder, may contribute to weight gain.
- Other factors: Scientists continue to search for other contributors to obesity. These may include the types and amount of good bacteria in your gut, cigarette smoking, and exposure to chemicals in your environment.
Don't feel discouraged if you're living with obesity. By speaking with a health care professional, you can start regaining control of your weight and your health.

Assessing Readiness
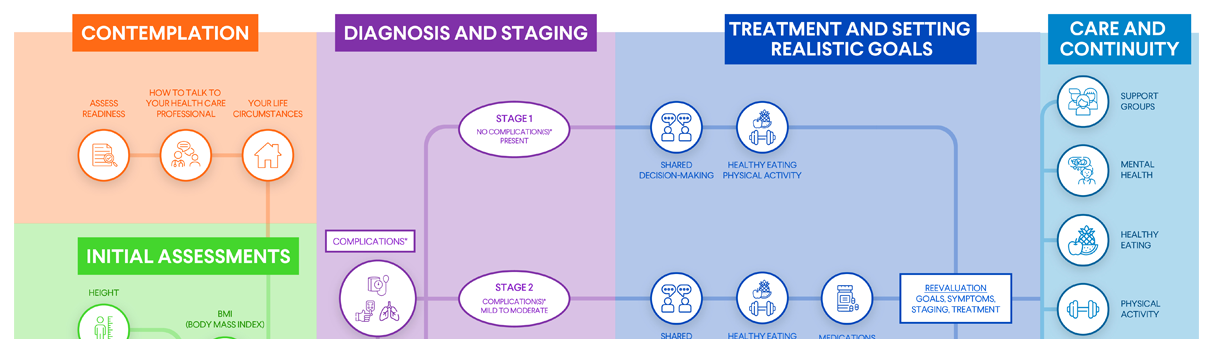
Your health care professional may use the "5A model" to support you on your obesity journey. This model was first developed to help people quit smoking, but its success led health care professionals to apply it to obesity as well.
As its name suggests, the 5A model incorporates five actions, all of which begin with the letter A. Here, we explain each of the five A's and how your health care professional may use them as you work together to manage your obesity.
The 5A Model
1. Ask
If you choose to discuss your weight with your health care professional, they may ask you about topics such as:
- Your understanding of the health impacts of obesity
- Whether your weight is affecting your quality of life
- Whether you're interested in losing weight
Keep in mind that your health care professional shouldn't be the only one asking questions during your appointments. You should ask questions, too. Feel free to write down a list of questions before your visit so you don't forget any. And take notes so you can remember your health care professional's answers.
If you think of any other questions when you get home, be sure to follow up with your health care professional.
2. Assess
Next, your health care professional will assess your physical and emotional health as they relate to your weight. This assessment includes various check-ins and measurements that seek to quantify the impact of obesity on your health and well-being, such as your:
- Weight
- Body mass index (BMI)
- Waist circumference
- Weight-related health complications
- Stage of obesity, which describes the severity of your complications
3. Advise
After the assessment, your health care professional will advise you on your treatment plan. Common options include:
- Setting goals
- Changing your eating habits
- Becoming more active
- Receiving behavioral counseling
- Consulting with other types of health care professionals
- Taking prescription medication
- Considering surgical procedures
4. Agree
This part of the 5A model is very important — and one you should be sure you understand. When your health care professional advises you on goals and a treatment plan, it's your choice whether to agree with those recommendations. It's your right to engage in shared decision-making with your health care professional. That means working together on a plan that meshes their advice with your preferences.
If you don't agree with what your health care professional suggests, let them know. Share what makes you uncomfortable, and work together to adjust the plan so that it meets your needs. Remember: It's your body, and shared decision-making is going to be important in deciding what treatment plan is best for you.
5. Assist
Once a treatment plan for managing your obesity is in place, your health care professional will assist you with your treatment. This may include actions such as:
- Creating a healthy eating plan
- Brainstorming ways to overcome exercise obstacles
- Looking at other factors that may impact your weight, such as poor sleep, cravings, and mood disorders, and recommending ways to manage them
- Periodically evaluating the effectiveness of your treatment plan and recommending adjustments as needed
- Referring you to a bariatric/metabolic surgeon
Along the way, be proactive and honest in letting your health care professional know what you need in terms of resources and support. Your health care professional cannot make appropriate recommendations without honest information. Be sure to share if you are struggling with your plan, are not able to reach your goals, or have any other concerns. Through open communication and shared decision-making, you can work together to reassess your goals, refine your treatment plan, and fine-tune any strategies that aren't working as well as they could be.
By following the 5A model, your health care professional can help you define and achieve your obesity management goals so you can improve your health and quality of life.
Your Life Circumstances
Your personal life circumstances can make you more or less likely to develop obesity. Where you are born, live, learn, and work all affect your health, well-being, and quality of life. As mentioned above, these factors are referred to as social determinants of health (SDOH).
The federal government groups SDOH into five categories:
- Economic stability: Do you have steady, well-paying work? Can you afford the food and other items you need to stay healthy?
- Education access and quality: Are high-quality educational opportunities available where you live? Can you afford a college education for yourself or your children?
- Health care access and quality: Do you have health insurance? Are you receiving all the health care services you need?
- Neighborhood and built environment: Do you live somewhere with high rates of violence? Is your drinking water safe? Can you easily access nutritious foods?
- Social and community context: Do you regularly face racism or discrimination? Do you have the support of others when times are tough?
In many lower socioeconomic communities, SDOH raise the risk of obesity and other health problems. For example, eating healthy foods can be challenging if you live in poverty. Having inadequate or no health insurance can mean a health care professional isn't looking after you. Living somewhere without parks or sidewalks makes it harder to be physically active.
If your life circumstances are creating issues that could put your health at risk, let your health care professional know. That will allow them to take steps to help keep you healthier.
Did You Know?
Obesity and Chronic Disease
- Ninety-six million Americans — about 38% of the U.S. population — have prediabetes, which means their blood sugar is higher than normal but not yet high enough for a diagnosis of type 2 diabetes. Losing weight can reverse prediabetes and can postpone or prevent the development of type 2 diabetes.
- For some people with type 2 diabetes, significant weight management (through lifestyle changes or surgery) can bring blood sugar levels down into the non-diabetes range and may lead to remission.
- Losing as little as 10 pounds can lower your blood pressure.







 DOWNLOAD
DOWNLOAD