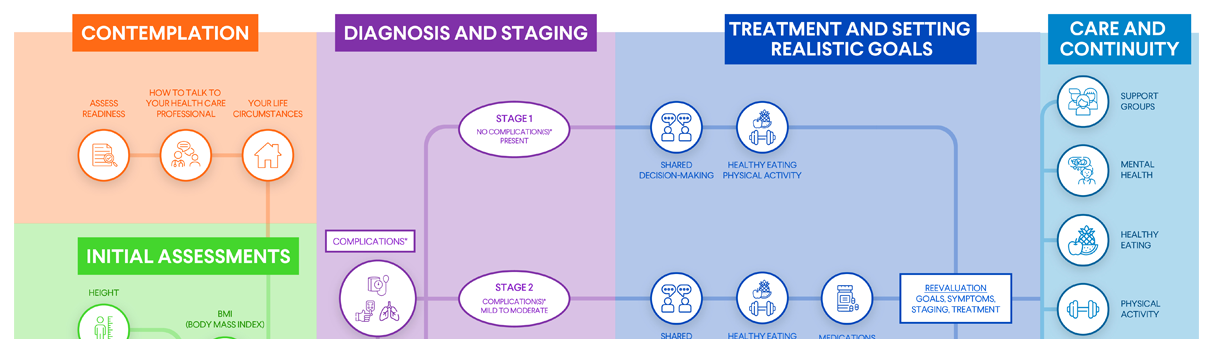
Treatment and Goals
Planning and Treatment, Stage 2

Planning and Treatment, Stage 2
Stage 2 obesity means you have one or more mild to moderate weight-related complications. In other words, you have both obesity and at least one medical condition that may affect your health.
The treatment goals for stage 2 obesity are to:
- Reduce your weight.
- Improve your weight-related health condition(s).
- Prevent other chronic health conditions from occurring in the future.
Losing weight can also reduce your risk of developing obesity-related complications and many types of cancer, including breast cancer, colorectal cancer, and prostate cancer.
Making lifestyle changes is important if you have stage 2 obesity. Besides helping you lose weight, taking steps such as improving your eating habits and engaging in physical activity can improve your overall health and lower your risk of developing weight-related conditions and chronic diseases.
Stage 2 obesity treatment typically includes taking steps to reduce chronic disease risk and changing your behavior habits. Key treatment strategies are:
- Setting realistic weight management goals
- Healthy eating
- Physical activity
- Weight management medications
Learn more about each treatment strategy below.
Setting Realistic Weight Management Goals
At the beginning of your obesity journey, try setting a modest goal — say, loss of 5%-10% of your body weight over the course of six months. This amount of weight loss has been shown to provide benefits in many obesity-related complications, including diabetes, high blood pressure, and non-alcoholic fatty liver disease. Once you meet that goal, you and your health care professional can set a new one.
Losing a lot of weight may require setting new goals multiple times. By working with your health care professional, you can establish realistic goals that will produce results and motivate you to succeed.
Healthy Eating
Eating a healthy diet that includes nutrient-rich foods in right-size portions is one of the best changes you can make for your weight and health.
Keep the following tips in mind as you think about healthy eating — and be sure to ask your health care professional for whatever guidance and support you need.
- What to eat: A healthy diet includes a wide range of nutritious foods, including fruits, vegetables, whole grains, lean meats, poultry, eggs, seafood, low-fat dairy, nuts, seeds, legumes, and healthy fats.
- What to avoid: A healthy diet limits highly processed foods; sugar-sweetened beverages; alcohol; and foods with added sugar, saturated fats, trans fats, or sodium.
- Portion control: No matter how healthy your diet is, you'll lose weight only if you eat the correct number of right-size portions. A good source of information about portion control is the U.S. Department of Agriculture's MyPlate Plan.
- Calorie control: For slow, steady weight loss, many health care professionals recommend reducing daily calorie intake by 500-750 calories. You and your health care professional can decide together how many calories you need each day. In a typical healthy eating plan, total daily calorie goals that include a reduction in calories for weight loss range from 1,200-1,600 for women and 1,500-1,800 for men. However, this varies for each person.
If you're currently following a calorie goal but not achieving any weight loss, you're taking in too many calories to lose weight. Your health care professional may recommend cutting your daily calories by an additional 100-200 calories. Your height, starting weight, and activity level all help determine what your daily calorie intake should be.
Meal plans to follow: Let your health care professional know if you'd like to follow a specific meal plan. Good options include the Mediterranean diet, the Dietary Approaches to Stop Hypertension (DASH) eating plan, and the MyPlate Plan.
Your health care professional may also recommend other types of eating plans, such as a low-carbohydrate or low-fat food plan, a low-calorie/high-volume food plan, a high-protein food plan, vegetarian eating, intermittent fasting, or a plan that substitutes some of your meals with meal-replacement drinks. Each of these plans has different pros and cons. Your health care professional can recommend the plan that's best for you.
A very-low-calorie diet is an option for some individuals, but it requires medical supervision and should be followed only if your health care professional recommends it.
Need extra support? Ask your health care professional to refer you to a registered dietitian or health educator.
Physical Activity
Increasing your physical activity burns calories and speeds up weight loss. It provides many other benefits, too, such as lower blood pressure, improved cholesterol levels, better heart health, stronger bones and muscles, better sleep, and improved mood. By getting moving, you help yourself in multiple ways.
Your health care professional will give you guidance on how much exercise you can do, what types of activities are best for you, and what types of exercise to avoid because of physical limitations or other factors.
Keep the following tips in mind as you think about physical activity — and be sure to ask your health care professional for whatever guidance and support you need.
- How much exercise to do: Any amount of exercise can benefit your health. But the general recommendation for physical activity is:
- 150 minutes per week of moderate-intensity physical activity (e.g., walking, swimming, biking, or playing tennis).
- Two days per week of muscle-strengthening activity that works all major muscle groups (i.e., legs, hips, back, abdomen, chest, shoulders, and arms). Strength training builds muscle mass, which contributes the most to metabolic rate. It's also very important for bone health.
- How to get started: It's fine to start with short bouts of activity and to increase duration over time. Start with something simple, such as walking a few minutes a day. As you become fitter, you'll be able to increase your walking distance and intensity. About 30 minutes a day, five days a week, is recommended. Alternatively, you could exercise for a longer duration on fewer days. Keep in mind that you can break up your activity into several shorter sessions throughout the day.
- Pick something you enjoy: You're more likely to stick with activities that you enjoy. No interest in jogging? No problem. Walk, hike, dance, play pickleball, or take a Zumba class instead.
- Work activity into your everyday life: Spending time with a friend? Go for a walk instead of a meal. Watching TV? Lift some weights while you watch. And your dog will love it if you start taking them out for extra walks.
- Track your progress: Using a step counter or other tracking tool may help you stay committed to exercise. The standard recommendation is 10,000 steps a day, but don't feel you have to start with that many steps. Begin with what feels doable, and gradually increase your daily step count goals over time.
- Join a gym — or not: Lots of people enjoy exercising at a gym, working out with a trainer, or participating in group exercise classes. But that doesn't mean you have to invest in a gym membership if you're not a fan of gyms. All you need to get started is a comfortable pair of shoes and a place to walk. You could also check out the many free exercise classes available online.
- Reduce sedentary behavior: Have a job that requires long hours of sitting? Try to schedule frequent breaks throughout the day to stretch or walk around, even if just for a couple of minutes.
Need extra support? Ask your health care professional to refer you to a physical therapist or medical exercise program.
Weight-Management Medications
Recommendations for weight management tend to focus on behavioral/lifestyle changes like healthy eating and physical activity. However, some people with obesity need something more.
If you have stage 2 or stage 3 obesity, your health care professional may bring up the possibility of taking prescription weight-management medications. Medicine cannot replace healthy eating and physical activity. But if you have certain weight-related chronic health conditions or have been unable to lose weight through other means, combining medicine with behavioral/lifestyle changes may help.
Consider this finding from the National Institutes of Diabetes and Digestive and Kidney Diseases: On average, after one year, people who combine prescription weight-management medications with lifestyle changes lose 3%-12% more of their starting body weight than people in a lifestyle program who do not take a medication.
Here's some information that can guide you in discussing weight-management medications with your health care professional.
How Weight-Management Medications Work
Weight-management medications come in both oral and injectable forms, but it's crucial to understand the correct dosage for each. The FDA has reported that overdoses can happen due to incorrect dosing, particularly with compounded medications. To ensure your safety, always consult your health care professional about the appropriate dosage for you.
Side Effects
Most medications cause side effects (unintended, often negative, reactions in your body). Side effects may be temporary or permanent. They may be minor or serious, or anywhere in between.
When studying medications, researchers keep track of the side effects that occur in people who take them. The common side effects must be included on the medication's package label.
It's important to ask your health care professional about the common side effects for any medications you're considering. Having this information can help you decide whether you want to take the medication and what to expect if you take it.
Common side effects of weight-management medications include:
- Headaches
- Nausea
- Abdominal pain
- Frequent bowel movements
- Constipation
- Diarrhea
- Dry eye
- Dry mouth
- Anxiety
- Depression
- Mood swings
- Dizziness
- Vomiting
- Increased heart rate
- Insomnia
Keep in mind that people respond to medications in different ways, so side effects can vary from person to person.
In addition, some medications may cause more serious side effects in people who have certain medical conditions or take certain other medications. Be completely open with your health care professional about your medical history and any medications or supplements you're taking. Your health care professional will let you know what kind of testing or monitoring you may need to watch for serious side effects.
If you take a weight-management medication and experience a side effect, tell your health care professional. Depending on the type and seriousness of the side effect, your health care professional may:
- Wait to see if the side effect lessens or stops.
- Recommend comfort measures or medications to help you cope (e.g., over-the-counter eyedrops for dry eye).
- Change your medication dose.
- Take you off the medication.
- Switch you to another medication.
Length of Treatment
As you and your health care professional discuss weight-management medications, be sure you understand how long you will stay on the medication. Some drugs should be taken only for a short time, while others are safe for longer periods of time. You should also understand whether you should expect to gain weight when you stop taking the medication.
Setting Realistic Expectations
Your health care professional can help you set realistic expectations about how much weight you may lose while taking a weight-management medication. Different drugs have different success rates, and people respond to drugs differently. Generally, people who take weight-management medications may expect to lose 5%-20% or more of their starting weight. But your results will depend on many factors, including starting weight, age, activity level, eating habits, stress levels, and sleep habits.
Medication Costs
Before choosing a weight-management medication, check with your health insurance carrier about your out-of-pocket costs.
FDA-Approved Medications for Adults With Obesity
The U.S. Food and Drug Administration (FDA) has approved five weight-management medications for long-term use. Please note: You won't find comprehensive lists of side effects for the medications below. Be sure to ask your health care professional about all side effects that could affect you.
- Phentermine/topiramate (Qsymia®): This is a capsule that decreases your appetite and helps you feel full after eating. Side effects may include headache; dizziness; trouble concentrating; tiredness; change in taste; a racing heart; and numbness or tingling in your arms, face, feet, and hands. It may not be taken with certain antidepressants or if you have glaucoma, an overactive thyroid, or certain heart or mental health conditions.
- Naltrexone/bupropion (Contrave®): This is a tablet that reduces your appetite to help you eat less. It's also used to help people stop smoking. People who have seizure disorders or take opioid medications should not take it. Since it can affect your heart, your health care professional will monitor your heart rate and blood pressure for the first 12 weeks. Side effects may include headache, dry mouth, constipation, nausea, vomiting, and, rarely, suicidal thinking.
- Liraglutide injection (Saxenda®): This medicine, injected once daily, reduces appetite and helps you feel fuller by slowing down stomach emptying. It's also prescribed to treat diabetes because it enhances your body's ability to produce insulin. Side effects may include nausea, vomiting, diarrhea, abdominal pain, constipation, injection-site rashes, and suicidal thinking.
- Semaglutide injection (Wegovy®): This drug has a similar mechanism of action as liraglutide but is injected once a week. It reduces your appetite and helps you feel fuller by slowing down stomach emptying. It's also prescribed to treat diabetes because it enhances your body's ability to produce insulin. Side effects may include nausea, vomiting, diarrhea, abdominal pain, heartburn, constipation, burping, suicidal thinking, and injection-site rashes.
- Orlistat (Xenical®, Alli®): Orlistat is a capsule that blocks the absorption of one-third of the fat in the foods you eat. It tends to be most effective for people who eat a high-fat diet. Side effects may include oily stools, stool leakage, loose stools, urgent bowel movements, stomach pain, gas, cramps, and irregular periods in women. Your health care professional may recommend vitamin supplements, because orlistat can reduce your body's ability to absorb certain nutrients from food.
- Tirzepatide (Zepbound™): Tirzepatide is a weekly injection that helps you eat less. It works by activating hormone receptors related to appetite. It has been approved by the FDA in adults with obesity or overweight and at least one weight-related health condition, such as type 2 diabetes, high blood pressure, or high cholesterol. Tirzepatide is also prescribed under the name Mounjaro® to help improve blood sugar in people with type 2 diabetes. Side effects may include nausea, diarrhea, vomiting, constipation, abdominal pain, indigestion, injection site reactions, fatigue, allergic reactions, belching, hair loss, and gastroesophageal reflux disease. Tirzepatide causes a type of thyroid tumor in rats, but researchers don’t know if it causes that type of tumor in humans.
Visit the FDA for more information about drug compounding.
Other Weight-Management Treatments
- Meal-replacement shakes replace meals with specially designed drinks.
- Pre-packaged meal replacement plans have specified amounts of calories and macronutrients. Meals can be purchased through various meal plans or can be made independently.
- Phentermine (Adipex®, Lomaira®, and Suprenza®) is an amphetamine-like pill that stimulates your central nervous system and decreases your appetite. It is only FDA-approved for a limited amount of time, depending on the state you live in (most common is three months or less).
Other promising weight-management therapies will become available in the future. For example, researchers are looking at medications that could bring about weight loss by altering gut hormones or gut bacteria. They're also investigating treatments that could change the action of certain genes related to obesity — a process known as gene editing.
Choosing the Right Medication for You
Once you and your health care professional have talked about your weight-management medication options, common side effects, and the results you can realistically expect to see, you can choose how to proceed. Don't feel pressured to make a quick decision — it's okay to take time to consider everything you and your health care professional have discussed.
Shared Decision-Making
You and your health care professional will work together to create a personalized treatment plan that's right for you and lets you manage your weight in a healthy way. Once you begin treatment, you and your health care professional can keep in touch to assess your progress and make any necessary treatment adjustments.
Note: Obesity pharmacotherapy, metabolic and bariatric surgeries, and metabolic endoscopic procedures may be considered at any stage of obesity, including stages 1 and 2. Treatment decisions should be made through a shared decision-making process between you and your health care professional. These interventions can be appropriate at any stage to support your lifestyle goals and improve your overall health.



 DOWNLOAD
DOWNLOAD